What is Total Hip Replacement (Arthroplasty)?
Total hip replacement surgery removes damaged bone and cartilage from a painful hip and replaces it with a prosthetic or artificial hip.
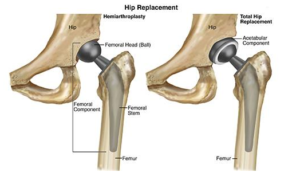
The hip joint is a ball-and-socket joint. The ball is part of the femur (thigh bone) and the socket is part of the hip bone/pelvic bone. The type of hip replacement surgery performed varies with each individual’s physical condition.
The 2 types of hip replacement surgeries are:
Total hip arthroplasty
With total hip arthroplasty, the ball and the socket are both replaced with artificial parts. Total hip arthroplasty is performed to treat conditions, including osteoarthritis, rheumatoid arthritis,
- traumatic arthritis,
- ankylosing spondylitis,
- avascular necrosis,certain hip fractures, and
- benign and malignant tumors.
Hemiarthroplasty
With hemiarthroplasty, or partial hip replacement, only the ball is replaced. Hemiarthroplasty is performed when there is damage only to the femoral portion of the hip joint. This is mostly performed in patients who are elderly and frail, and for fractures involving the ball or the neck of the femur (thigh bone).
 How Can a Physical Therapist Help?
How Can a Physical Therapist Help?
Before Surgery
Your physical therapist can help educate youabout what to expect from your surgery, and give you exercises to condition your body presurgery.
In preparation for surgery, your physical therapist may teach you:
- Flexibility and strengthening exercises for the lower extremities
- How to use a walker or crutches for walking and for navigating steps
- Any precautions to take after surgery
After surgery, your physical therapist may tell you not to:
- Bend your new hip more than 90 degrees.
- Bend forward more than 90 degrees. (For example, you will not be able to bend over to put on your socks and shoes for a while.)
- Cross your leg with your new hip over the other leg.
- Turn the leg with the new hip inward.
Your therapist may recommend changes in your home to improve safety and help your recovery, including the use of a raised toilet seat, hand rails on stairs, a bed rail, and a tub seat or grab bars in the shower.
It is recommended that you make these changes before you have surgery, so your home is prepared for your return.
After Surgery
On the first or second day after your surgery, your physical therapist will come to your bedside to begin your postoperative treatment. Your therapist will review any postsurgical precautions to take to prevent reinjury and to help restore your full function.
During your acute-care recovery (the first 3–5 days after surgery), your physical therapist will work with you to help you safely:
- Turn in bed and get up to a sitting position
- Get out of bed to stand and move to a chair
- Walk with an assistive device (walker or crutches) for short distances
- Perform gentle range-of-motion and strengthening exercises in bed
Physical Therapy will continue during your subacute recovery (4–6 weeks). You may need to recover in a short-term rehabilitation facility. Some patients are discharged to their home without nursing-home care, depending on the help available at home and their ability to stay safe. Your physical therapist will help make this determination for you.
As you progress in your recovery, you will continue to work on:
- Walking and stair climbing.
- Balance—after surgery your balance may be impaired, which could put you at risk for falls.
- Transferring to the bed, a chair, and a car.
- Full movement of your leg and new hip (such as putting on socks and shoes).
- Specific muscle strengthening exercises to improve your ability to stand and walk safely and independently.
When you are independent in these activities you will be ready to fully function at home. However, you may still need to continue physical therapy in an outpatient clinic.
Outpatient physical therapy sessions will continue your work on range of motion and stretching exercises, and weight-bearing activities to restore your function to optimal levels. This level of physical therapy focuses on activity-specific rehabilitation for your specific goals, such as a return to work or sport. Your physical therapist will incorporate exercises that simulate those activities. These may include lifting techniques, pushing, pulling carts, climbing ladders, agility exercises, or light jogging depending on your recovery and activity level.
How Does it Feel?
Before surgery, patients may experience severe pain in the hip and groin, and occasionally down the thigh. They may also have significant difficulty walking, navigating stairs, and sleeping on the affected side.
Postsurgery
After total hip replacement surgery, you will experience stiffness in the hip and leg, and muscle weakness. Postsurgical pain is expected for an average of 4 to 6 weeks. However, some patients may experience pain for up to 12 weeks, or even longer.
Pain is managed primarily with medication. Your physical therapist may also recommend ice packs to help reduce discomfort.
It may be difficult to put weight on your leg when walking after surgery. Depending on your particular case/surgical procedure, you will be asked to limit the amount of weight you put on the surgical leg. It may be as little as a toe touch, or as much weight bearing as you can tolerate. Your physical therapist will teach you how to correctly put weight on the affected leg, and will recommend an assistive device, such as crutches or a walker to minimize discomfort as you work to restore your physical function.
How Is It Diagnosed?
When you seek help for hip pain, you will be evaluated by a medical professional. Your doctor will order hip x-rays to assess whether there is damage to the hip. A physical therapist will evaluate your functional mobility, such as how you get in and out of bed, stand up from sitting in a chair, and walk. The results of these evaluations will help determine whether you need total hip replacement surgery.
Hip replacements are most often performed in adults aged 60–80. Your doctor will determine if you are a good candidate for surgery based on your x-rays and your physical assessment. The doctor will also consider risk factors that may interfere with your recovery, such as advanced age, obesity, or a history of smoking or excessive alcohol intake.
