What is Total Shoulder Arthoplasty?
Total shoulder arthroplasty is a surgical procedure in which part or all of the shoulder joint is replaced. It is performed on the shoulder when medical interventions, such as other conservative surgeries, medication, and physical therapy no longer provide pain relief. The decision to have a TSA is made following consultation with your orthopedic surgeon and your physical therapist.
A shoulder replacement may be needed if you have any of the following conditions affecting the shoulder, causing severe shoulder pain and limiting your ability to use the affected shoulder:
- Osteoarthritis
- Rheumatoid arthritis
- Severe shoulder fracture
- Rotator cuff disease (a muscle tear or soft-tissue breakdown of the rotator cuff)
- Osteonecrosis of the shoulder (death of the bone tissue at the head of the humerus)
A TSA involves removing the ends of the bone at the shoulder joint, and replacing them with artificial parts.
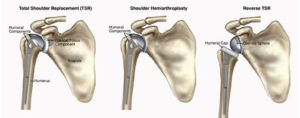
The upper part of the arm bone (humerus) is shaped like a ball; it is called the “head” of the humerus. During a TSA, the head of the humerus is replaced by a metal ball. The socket that the head of the humerus sits in is called the glenoid fossa. During a TSA, the socket is replaced by a plastic cup.
Due to various physical limitations, your orthopedic surgeon may decide that you are a candidate for another form of TSA, such as:
Shoulder hemiarthroplasty, where only the head of the humerus is replaced with a metal ball.
Reverse TSA, where the metal ball and plastic socket are reversed. This procedure is recommended when the rotator cuff muscles of the shoulder are damaged. The plastic socket is attached to the top of the humerus, and the metal ball is attached to the socket. This procedure allows another shoulder muscle, called the deltoid, to take over for the damaged rotator cuff muscles, improving functional range of motion, strength, and stability of the shoulder
Back to Top
How Can Physical Therapy Help?
Physical therapy plays a vital role in ensuring a safe recovery by improving shoulder function, and limiting pain following a TSA. Your physical therapist will work with you prior to and following your surgery, to help you safely return to your previous levels of activity, including performing household chores, job duties, and recreational activities.
Before Surgery
The better physical condition your shoulder is in prior to surgery, the better your recovery will be. Your physical therapist will teach you exercises to build shoulder strength, and improve your shoulder and upper back movement to keep the shoulder as strong and mobile as possible up until the time of surgery.
After Surgery
Your physical therapist will educate you about precautions to take after surgery, such as wearing a sling to perform all activities, and gradually beginning to safely move your arm. If you are a smoker, quitting smoking will improve your healing process.
After your TSA, you will likely stay in the hospital for 2 to 3 days. If you have other medical conditions, such as diabetes or heart disease, your hospital stay may be a few days longer. Your shoulder will be placed in a sling for the next 2 to 6 weeks; you will be advised to not move your shoulder on your own.
Your physical therapy will begin within a day or two of your surgery. A hospital physical therapist will visit your room to teach you how to perform simple tasks like brushing your teeth, and tell you what movements (such as pushing, pulling, or reaching with the affected arm) you simply cannot perform. Your physical therapist will teach you how to get in and out of bed safely, how to get the sling on and off, and how to get dressed while keeping your shoulder in a safe position. You will also learn how to minimize pain and swelling in the area by applying an ice pack, and elevating the upper arm.
You may need some help from friends or family members with daily activities for the first few days or weeks after your surgery. You will not be able to drive for the first few weeks after surgery.
As You Recover
When you are discharged from the hospital, continuation of physical therapy is essential. Your surgeon and physical therapist will work as a team to ensure your safe recovery. Your physical therapist will teach you exercises that may include:
Range-of-Motion Exercises. It is important to not move your shoulder suddenly or with any force for the first 2 to 6 weeks following surgery, to allow proper healing. Your physical therapist will passively move your shoulder in different directions to allow you to safely begin regaining movement. Your physical therapist will also teach you gentle exercises to perform at home. You will also learn range-of-motion exercises for the elbow and hand, so these joints do not get stiff from being held in a sling. Squeezing a ball or putty will help keep your grip strong, while your shoulder recovers. You will use ice packs on the shoulder and elevate your arm on pillows to allow gravity to help reduce the swelling in the shoulder, as instructed by your physical therapist.
Strengthening Exercises. As your shoulder mobility returns within a few weeks or months, your physical therapist will guide you through a shoulder strengthening program. You may use resistive bands and weights to perform gentle strengthening exercises.
Functional Training. Your physical therapist will help you regain everyday shoulder movements, such as reaching into a cupboard, reaching behind your body to tuck in your shirt, or reaching across your body to fasten a seat belt.
Job and Sport-Specific Training. Your physical therapist will design a personalized program to enable you to resume your job tasks without pain. These may include reaching, pushing, or carrying movements. You will also receive sport-specific training if you are planning to return to a sport. Your physical therapist will create a specialized home or fitness-center exercise program based on your individual needs, to be continued long after formal physical therapy has been completed.